Did you know that a splenectomy, the surgical removal of the spleen, is often a critical intervention for rare blood disorders like idiopathic thrombocytopenic purpura, where platelet counts plummet dangerously low? As you consider this procedure, whether due to trauma or chronic illness, you’ll find that its implications—ranging from infection risks to improved quality of life—span a complex medical landscape. Explore how this surgery could impact your health journey.
Key Takeaways
- Splenectomy is a surgical procedure to remove the spleen, often treating hematologic disorders like idiopathic thrombocytopenic purpura.
- Costs vary widely: $3,000–5,000 in India, compared to $15,000–25,000 in the United States.
- Laparoscopic splenectomy uses small incisions, offering shorter hospital stays and faster recovery.
- Post-surgery care includes antibiotics, vaccinations, and regular follow-ups to prevent infections.
- Risks persist, including severe infections, requiring ongoing precautions and lifestyle adjustments.
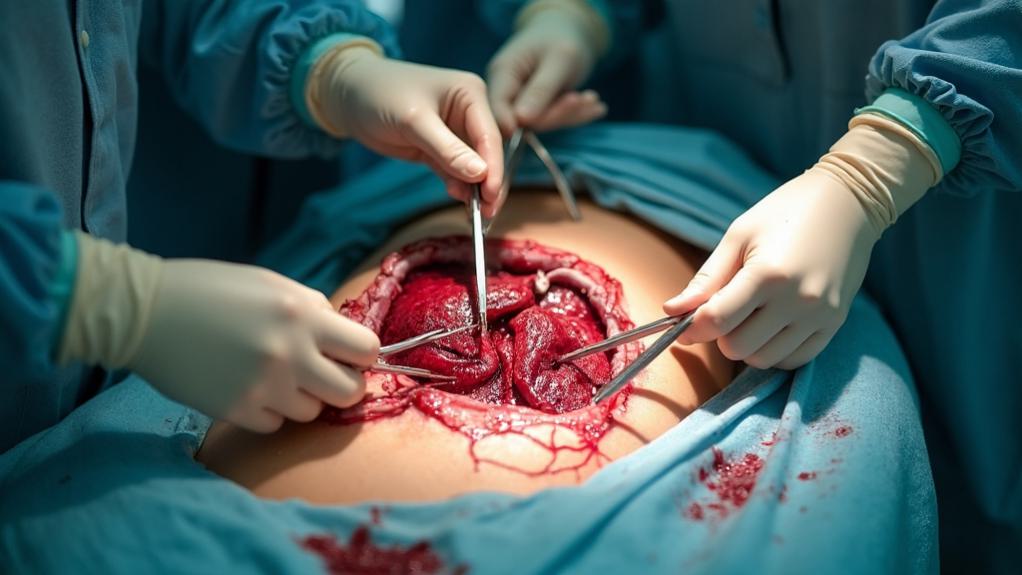
Splenectomy, the surgical removal of the spleen, stands as a critical procedure often necessitated by trauma, hematological disorders, or severe infections, yet it carries a spectrum of risks that demand careful consideration. As you navigate the decision to undergo this surgery, whether elective or emergent, you must weigh the immediate benefits against potential postoperative complications that could profoundly impact your health. Infections, for instance, rank among the most prevalent concerns, manifesting as wound infections, abscesses, or even life-threatening conditions like sepsis and pneumonia, while lower respiratory tract infections and intra-abdominal collections further complicate recovery. Beyond infections, you face the peril of acute haemorrhage, particularly if you suffer from severe splenomegaly, where excessive bleeding could necessitate urgent intervention.
Delving deeper into the surgical risks, you should be aware that injury to adjacent organs, such as the pancreas, can occur during the procedure, potentially leading to long-term complications like pancreatic fistulas or chronic pain. Additionally, venous thromboembolism, including deep vein thrombosis and pulmonary embolism, poses a significant threat, as studies have consistently highlighted elevated risks post-splenectomy due to conditions like leukocytosis and thrombocytosis. A specific study from North India, for instance, reported complications such as acute renal failure, wound infections, and subphrenic abscesses among patients, though, particularly, no cases of overwhelming postsplenectomy infection (OPSI) emerged during follow-up. Furthermore, the loss of memory B cells post-splenectomy increases vulnerability to infections like pneumococcus and tetanus, emphasizing the importance of timely vaccinations memory B cells loss. These findings underscore the diverse spectrum of postoperative challenges you might encounter, ranging from pulmonary and hemorrhagic issues to infectious and thromboembolic events. Moreover, the study highlighted that adherence to postsplenectomy guidelines, particularly regarding vaccination and prophylaxis, was unsatisfactory, emphasizing the need for better enforcement to prevent infections guidelines adherence unsatisfactory.
To mitigate some of these dangers, you’re strongly advised to adhere to preventive measures, such as receiving vaccinations against pneumococci, meningococci, and Haemophilus influenzae, typically administered 14 days before elective surgeries or within 3 days for emergencies, to guard against OPSI. Additionally, long-term complications like splenosis, where ectopic splenic tissue deposits in the peritoneal cavity, or paralytic ileus, which disrupts intestinal movement and risks bowel obstruction, warrant your vigilance. As you contemplate this procedure, understanding these multifaceted risks—backed by clinical data and regional studies—equips you to engage in informed discussions with your healthcare providers, ensuring that every precaution is meticulously considered to safeguard your postoperative journey.
Overview
A splenectomy is a surgical procedure involving the removal of part or all of the spleen, an organ located in the upper left abdomen that plays a crucial role in filtering blood and supporting the immune system. While the spleen is not essential for survival, its removal may be necessary due to various medical conditions or injuries. Treatment options include laparoscopic splenectomy, a minimally invasive approach with smaller incisions and quicker recovery, and open splenectomy, a more invasive method often used in emergencies that involves a larger incision and longer recovery time. This procedure may be required for individuals who have experienced trauma to the spleen, suffer from hematologic disorders like sickle cell anemia or thalassemia, have an enlarged spleen (splenomegaly), or have tumors within the spleen. Both elective and emergency splenectomies are performed under general anesthesia to address these critical health concerns. Additionally, patients should be aware that recovery time can vary, often taking a few weeks to up to six weeks depending on the surgical method used with quicker recovery after laparoscopy. Post-splenectomy, patients require careful monitoring to manage potential infection risks due to the spleen’s role in fighting infections.
Treatment Details and Key Information
Splenectomy, the surgical removal of the spleen, is a well-established procedure offered in leading corporate hospitals across India, catering to foreign patients with world-class facilities, experienced surgeons, and advanced technology. These hospitals provide thorough care, including pre-operative assessments, personalized treatment plans, and post-operative support, often with dedicated international patient services to assist with travel, accommodation, and language barriers. The procedure typically takes about 1 to 2 hours, depending on the technique used and the patient’s condition. Hospital stay varies from 1 to 3 days for minimally invasive methods like laparoscopic or robotic-assisted splenectomy, while open surgery may require 5 to 7 days. Total recovery time generally ranges from 2 to 6 weeks, with laparoscopic and robotic approaches offering quicker recovery (2-4 weeks) compared to open surgery (4-6 weeks). The spleen plays a crucial role in fighting infections and filtering blood, but other organs compensate after its removal, though this increases the risk of infections. Patients undergoing splenectomy for conditions like a ruptured spleen often require immediate surgery to address life-threatening internal bleeding immediate surgery required. The types of procedures available include open splenectomy, which involves a larger incision and is suitable for complex cases or enlarged spleens but has a higher risk of complications and longer recovery; laparoscopic splenectomy, a minimally invasive technique using small incisions, a camera, and specialized tools, offering reduced pain and faster recovery but may not be feasible for very large spleens; and robotic-assisted splenectomy, which provides enhanced precision and control, potentially reducing complications, though it is more expensive and may not be widely available. Each method has its pros and cons, and the choice depends on the patient’s specific condition, the surgeon’s expertise, and the hospital’s infrastructure.
Key Benefits & Advantages
Splenectomy, the surgical removal of the spleen, offers significant benefits and advantages, making it a preferred treatment option in India for various medical conditions. This procedure is often chosen to address medical emergencies like severe spleen injuries, manage blood disorders, treat cancers affecting the spleen, and alleviate chronic diseases such as splenomegaly. India stands out as a destination for splenectomy due to its world-class medical facilities, highly skilled surgeons, and advanced laparoscopic techniques that guarantee minimal invasiveness, reduced post-operative pain, and shorter hospital stays. The success rates for splenectomy in India are particularly high, with many hospitals reporting effectiveness in symptom relief and control of underlying conditions, thanks to cutting-edge technology and multidisciplinary care approaches. Additionally, the affordability of the procedure in India, combined with personalized post-surgery care and enhanced recovery protocols, makes it an attractive option for both domestic and international patients seeking improved quality of life. However, it is important to note that while splenectomy can be highly effective, it is not a cure for any underlying condition and should be considered after thorough risk assessment.
| Country | Average Cost of Splenectomy (USD) | Affordability Notes |
|---|---|---|
| India | 3,000 – 5,000 | Highly affordable with quality care |
| United States | 15,000 – 25,000 | Expensive due to high healthcare costs |
| United Kingdom | 10,000 – 18,000 | Moderately expensive with long waiting times |
| Singapore | 8,000 – 12,000 | Higher cost but advanced facilities |
| Thailand | 4,000 – 7,000 | Affordable with good medical tourism options |
Treatment Process
The treatment process for a splenectomy, the surgical removal of the spleen, involves several critical steps and preparations. Before the procedure, diagnostic tests such as blood work, imaging studies like ultrasound or CT scans, and a thorough medical history review are conducted to assess the spleen’s condition and the patient’s overall health, ensuring the surgery is necessary and safe. Pre-surgery preparations include fasting for a specific period, typically overnight, and discussing current medications with the healthcare team to adjust or stop certain drugs like blood thinners. Patients may also receive vaccinations against infections such as pneumococcal, meningococcal, and Haemophilus influenzae type b, as the spleen plays a key role in immunity, and these are often administered weeks before or after surgery based on individual circumstances. On the day of surgery, the patient is placed under general anesthesia. For a laparoscopic splenectomy, the surgeon makes three or four small incisions in the abdomen to insert a laparoscope and specialized instruments, using carbon dioxide to inflate the abdominal cavity for better visibility. In an open splenectomy, a larger single incision is made. The spleen is then carefully disconnected from surrounding tissues and blood vessels, removed, and the incisions are closed with stitches, staples, or surgical glue. Throughout the procedure, the surgical team monitors the patient to manage any complications, ensuring a safe and effective operation.
Expected Outcomes
Splenectomy is often an effective treatment for various conditions, including hematologic disorders like idiopathic thrombocytopenic purpura and hemolytic anemia, as well as trauma and certain malignancies such as leukemia and lymphoma. Patients can expect significant improvement in symptoms and, in some cases, enhanced survival rates, with positive outcomes reported in approximately 75% of cases involving autoimmune cytopenia in common variable immunodeficiency (CVID). The procedure, whether performed via open or laparoscopic methods, often results in shorter hospital stays and faster recovery with the latter approach. However, success rates and long-term effectiveness depend heavily on the underlying condition and the patient’s preoperative health status. While many patients without severe injuries or comorbidities recover well, there remains a persistent risk of severe infections post-surgery, necessitating lifelong precautions such as vaccinations and, in some cases, long-term antibiotic use to manage this risk.
After-Treatment Care & Recovery
After a splenectomy, patients require diligent after-treatment care and recovery practices to guarantee a smooth healing process. Post-treatment medical requirements often include medications such as pain relievers and, in some cases, antibiotic prophylaxis to prevent infections due to the increased risk following spleen removal. Vaccinations against pneumonia, influenza, Hib, and meningococci are typically recommended to bolster immunity. Regular follow-up appointments and periodic blood tests, including platelet counts, are essential to monitor for complications or signs of infection like fever or redness, with immediate medical attention advised for even minor illnesses. During the recovery phase, necessary precautions include daily washing of the incision area with warm, soapy water, avoiding baths in favor of showers, and refraining from using hydrogen peroxide or alcohol on the wound. Patients should avoid crowds for the first two weeks post-discharge, practice frequent hand washing, and steer clear of heavy lifting or strenuous activities until cleared by their surgeon. Lifestyle changes may involve gradual increases in physical activity, avoiding driving until approved by a healthcare provider, and taking stairs slowly with breaks. Additionally, patients should adopt habits to minimize infection risks, such as avoiding bites and maintaining regular healthcare check-ups to support long-term health.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC1770256/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4621170/
- https://www.maxhealthcare.in/procedures/splenectomy
- https://www.ijsurgery.com/index.php/isj/article/download/1610/1358
- https://www.tridhascholars.org/pdfs/a-study-on-perioperative-complications-of-splenectomy-in-emergency-elective-cases-a-short-term-prospective-observational-study-at-a-tertiary-referral-hospital-JOCCR-6-1144.pdf
- https://www.ncbi.nlm.nih.gov/books/NBK560824/
- https://my.clevelandclinic.org/health/procedures/14614-splenectomy
- https://www.mountsinai.org/health-library/surgery/spleen-removal
- https://healthy.kaiserpermanente.org/health-wellness/health-encyclopedia/he.splenectomy.ue4533
- https://en.wikipedia.org/wiki/Splenectomy