Imagine, if you will, a world where clouded vision no longer dims your future—a possibility made real through corneal transplant surgery. You’re likely aware that in India, this procedure addresses severe conditions like microbial keratitis or keratoconus, often performed via techniques such as penetrating keratoplasty. With success rates spanning 65-95%, as reported by major hospitals, what challenges and triumphs await you on this transformative journey? Explore further to uncover the intricate details.
Key Takeaways
- Corneal transplant treats severe corneal damage, often from microbial keratitis, restoring vision with success rates of 65-95%.
- Types include full-thickness penetrating keratoplasty and partial transplants like endothelial keratoplasty for specific corneal layers.
- Success is high, with up to 98% achieving near-perfect vision, especially with advanced techniques.
- Recovery varies, from weeks for partial transplants to a year for full-thickness procedures.
- India’s world-class facilities, like Apollo and Fortis, cater to global patients with advanced care.
Vision, a cornerstone of human experience, often hangs in the balance for those grappling with severe corneal damage, where a corneal transplant emerges as a critical intervention to restore sight. If you’re facing debilitating conditions like microbial keratitis, which ranks as a leading indication for this procedure in India, you might find yourself among the thousands seeking this life-altering surgery. With success rates ranging from 65% to 95%, depending on the specific technique and individual circumstances, you can approach this option with cautious optimism, knowing that a significant majority of recipients regain functional vision, as evidenced by a study reporting a 79.6% survival rate for first-time transplants after one year.
As you navigate the landscape of corneal transplantation in India, you’ll encounter a variety of procedural approaches tailored to specific needs. If your condition involves active keratitis, therapeutic penetrating keratoplasty (PKP), which accounts for 27-34% of transplants in the country, might be recommended to halt disease progression. Alternatively, if your primary goal is vision enhancement, optical PKP, comprising 45-50% of cases, could be your path forward. You might also consider endothelial keratoplasty, a technique witnessing a rise in adoption from 13% to 17% over six years, particularly for conditions affecting the cornea’s innermost layer. These options, supported by regional efforts in states like Andhra Pradesh, Telangana, Gujarat, Karnataka, Maharashtra, and Tamil Nadu, reflect a robust network of procurement and surgical expertise. Additionally, understanding the impact of risk factors, such as socioeconomic status or previous transplant failures, can help you prepare for potential challenges, as studies show a higher risk with lower socioeconomic status.
Furthermore, you should be aware of the logistical framework underpinning these interventions, such as the short-term storage techniques that preserve corneal tissue for up to 14 days, ensuring timely availability. Tissue utilization rates, varying from 22-28% for voluntary donations to up to 50% in hospital-based programs, highlight the challenges and disparities in access that you might face. As the Government of India aims to reduce blindness prevalence to 0.25 per 1000 cases by 2025, your access to this procedure aligns with a broader national mission. Moreover, with an estimated annual requirement of 100,000 corneal transplants in India to meet the current demand, the scale of need underscores the importance of expanding donor networks and eye banking facilities. By understanding these dynamics, you position yourself to make informed decisions, leveraging a system that, while imperfect, offers a tangible hope for restored vision through meticulous surgical intervention.
Overview
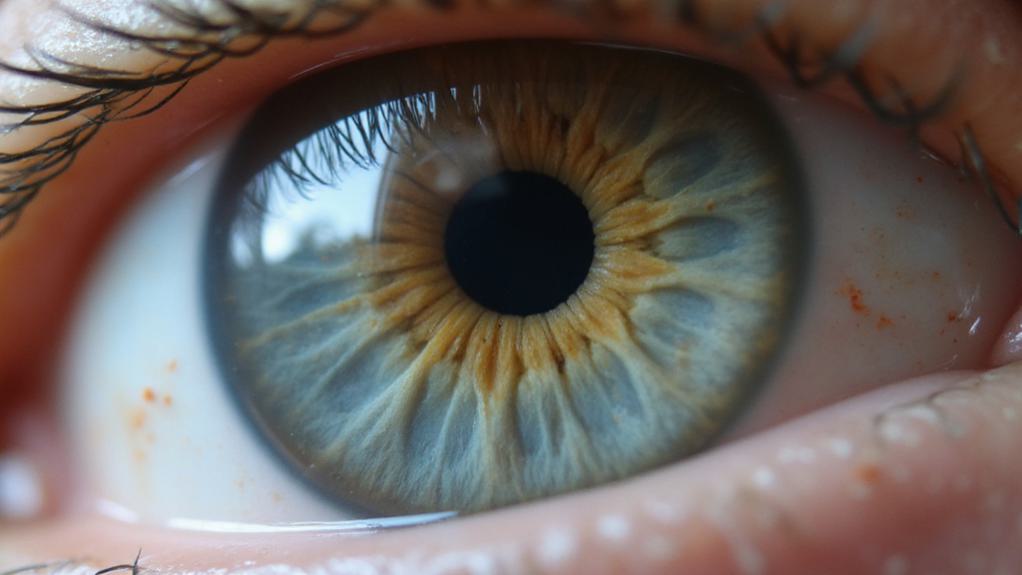
A corneal transplant, also known as keratoplasty, is a surgical procedure that involves replacing a damaged or diseased cornea with healthy donor tissue to restore vision and alleviate associated symptoms. The cornea, the clear front part of the eye, can become impaired due to conditions such as Fuchs’ dystrophy, keratoconus, corneal dystrophy, scarring from injury or infection, or complications from previous eye surgeries. Treatment options vary depending on the extent of damage and include full-thickness transplants, which replace the entire cornea, or partial transplants, which target specific layers of the cornea. This procedure is essential for individuals who experience significant vision loss or pain due to corneal damage that cannot be corrected with glasses, contact lenses, or other non-surgical interventions, ultimately improving their quality of life and preventing further complications. Over the years, techniques have evolved from traditional methods to advanced procedures like lamellar keratoplasty, focusing on selective tissue replacement for better outcomes. The success of these surgeries often depends on the body’s acceptance of the donor tissue, highlighting the importance of post-surgery care to minimize risks such as rejection.
Treatment Details and Key Information
Corneal transplant, a specialized eye surgery to replace damaged or diseased corneal tissue with healthy donor tissue, is widely performed in big corporate hospitals in India, such as Apollo, Fortis, and Max Healthcare, which cater to foreign patients with world-class facilities and internationally trained ophthalmologists. These hospitals offer thorough care, including pre-surgical evaluations, advanced surgical techniques, and post-operative support, often at a fraction of the cost compared to Western countries, making India a popular destination for medical tourism. The duration of hospital stay is typically minimal, with many procedures like endothelial keratoplasty (EK) being outpatient surgeries, allowing same-day discharge, while full-thickness penetrating keratoplasty (PK) may require a short stay of 1-2 days depending on the patient’s condition. Total recovery time varies—partial-thickness transplants like Descemet Membrane Endothelial Keratoplasty (DMEK) may see vision improvement within weeks, whereas PK can take up to a year for full recovery. The procedure itself usually lasts less than an hour, performed under local or general anesthesia based on patient needs. Various types of corneal transplant procedures are available, including Penetrating Keratoplasty (PK) for full-thickness replacement, which is effective for severe damage but has a longer recovery and higher risk of complications like graft rejection; Endothelial Keratoplasty (EK) variants like DSEK and DMEK, which target specific layers, offering faster recovery and lower rejection rates but requiring high surgical precision; and Deep Anterior Lamellar Keratoplasty (DALK), which preserves the patient’s endothelium, reducing rejection risk but is technically challenging. While robotic assistance is not typically used in corneal transplants due to the delicate manual nature of the surgery, advanced microscopes and tools enhance precision across all methods. Each technique has its pros and cons, with the choice depending on the specific corneal condition, patient health, and surgeon expertise. Success rates are generally high, with many patients benefiting from improved vision post-surgery. Most recipients of corneal transplants experience at least partial vision restoration after the procedure, though outcomes can vary based on individual health conditions and the reason for surgery.
Key Benefits & Advantages
Corneal transplant surgery stands out as a transformative treatment for individuals suffering from severe corneal conditions, offering a host of key benefits and advantages. In India, this procedure is increasingly preferred due to its high success rate of up to 98%, ensuring near-perfect vision restoration for many patients. The treatment not only reduces pain but also enhances the overall quality of life by providing long-term effectiveness, with many patients not requiring another transplant for over a decade. Additionally, India offers world-class medical facilities and highly trained ophthalmologists who utilize advanced surgical techniques, making it a top destination for this procedure. The versatility of corneal transplants, including options like partial transplants with lower risks and faster recovery, further adds to its appeal, alongside the durable outcome of improved vision clarity compared to temporary solutions like contact lenses.
| Country | Average Cost (USD) | Affordability Notes |
|---|---|---|
| India | 1,500 – 3,000 | Highly affordable with quality care. |
| United States | 13,000 – 27,000 | Expensive due to high healthcare costs. |
| United Kingdom | 8,000 – 15,000 | Moderately expensive with long waiting times. |
| Singapore | 5,000 – 10,000 | Moderate cost with advanced facilities. |
| Thailand | 2,500 – 5,000 | Affordable, popular for medical tourism. |
Treatment Process
The treatment process for a corneal transplant begins with thorough pre-surgery preparations and diagnostic evaluations to confirm the patient is a suitable candidate for the procedure. Initially, a detailed medical history review is conducted by the surgeon and anesthesia team to assess any underlying conditions or risks. Diagnostic tests, such as corneal topography and pachymetry, are performed to evaluate the cornea’s shape and thickness, helping to determine the specific type of transplant needed. Patients receive pre-surgery instructions, including guidelines on when to stop eating and drinking, and may be advised to adjust or discontinue certain medications. Transportation arrangements must also be made, as patients will be unable to drive after the procedure. On the day of surgery, the anesthesia type—planned in advance—is administered to minimize risks. The surgical technique varies depending on the condition: penetrating keratoplasty replaces the full thickness of the cornea with donor tissue secured by stitches; endothelial keratoplasty, such as DSEK or DMEK, targets only the innermost layer using an air bubble to position the tissue; and anterior lamellar keratoplasty replaces the outer layers while preserving the endothelium. Specialized instruments, like non-coapting forceps, are used to handle the delicate donor tissue, guaranteeing precision during the procedure.
Expected Outcomes
Patients undergoing corneal transplant surgery can generally expect significant vision improvement, with many experiencing clearer vision within months after the procedure, although initial blurriness is common during the early healing phase. Short-term success is high, with national graft survival rates reported at up to 88% at two years, and even patients over 90 years old achieving comparable outcomes at 12 months. However, long-term effectiveness varies, as graft survival rates decline over time, dropping to an estimated 27% at 20 years and just 2% at 30 years. Factors such as patient health, underlying conditions, and surgeon skill influence these outcomes, while risks like graft rejection, infection, and late complications can impact success. Continuous monitoring through regular follow-up appointments is essential to maintain graft health and address any issues that may arise over the years.
After-Treatment Care & Recovery
After a corneal transplant, proper after-treatment care and recovery are essential for a successful outcome. Patients are prescribed eye drops, including antibiotics and immunosuppressants, to aid healing and prevent rejection, and strict adherence to the dosage and schedule is essential. Regular follow-up appointments are essential to monitor vision changes, address potential complications like irritation or blurry vision, and guarantee the effectiveness of the medication regimen. During the recovery phase, precautions must be taken to protect the operated eye, such as wearing eye shields, especially at night, and avoiding water, soap, or chemicals near the eye while bathing or washing hair, which is permitted after 4 days with care. Activity restrictions include avoiding heavy lifting, bending, stooping, and strenuous exercise for about 4 weeks, while resting or lying on the back is often advised. Lifestyle changes may involve minimizing physical activities initially, resuming normal work and routines after 1 to 2 weeks depending on the transplant type, and potentially using contact lenses or glasses for best vision, as full recovery can take several months to a year or more.
References
- https://pubmed.ncbi.nlm.nih.gov/9422922/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10565946/
- https://journals.lww.com/transplantjournal/fulltext/2019/12000/high_risk_corneal_transplantation__recent.9.aspx
- https://journals.lww.com/ijo/fulltext/2023/71090/evolution_of_eye_banking_in_india___a_review.6.aspx
- https://www.cureus.com/articles/109003-a-review-of-corneal-transplantation-an-insight-on-the-overall-global-post-covid-19-impact.pdf
- https://www.ncbi.nlm.nih.gov/books/NBK539690/
- https://www.aao.org/eye-health/treatments/about-corneal-transplantation
- https://www.nhs.uk/conditions/cornea-transplant/what-happens/
- https://my.clevelandclinic.org/health/treatments/17714-cornea-transplant
- https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/corneal-transplantation
- https://www.mayoclinic.org/tests-procedures/cornea-transplant/about/pac-20385285
- https://www.upmc.com/services/eye/services/cornea/corneal-transplant
- https://www.nhs.uk/conditions/cornea-transplant/
- https://blog.nvdonor.org/blog/understanding-the-benefits-of-corneal-transplants
- http://sacramentoeyeconsultants.com/blog/what-is-corneal-transplant-treatment-and-who-can-benefit.html
- https://webeye.ophth.uiowa.edu/eyeforum/tutorials/cornea-transplant-intro/index.htm
- https://pubmed.ncbi.nlm.nih.gov/19815285/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10101946/
- https://www.healio.com/news/ophthalmology/20210311/good-outcomes-seen-after-corneal-transplantation-in-patients-older-than-90-years
- https://www.nhs.uk/conditions/cornea-transplant/recovery/